The study identifies five key factors that predict the response of cancer patients to immunotherapy
Credit: Unsplash/CC0 Public Domain
A team of IRB Barcelona researchers identified five independent factors that predict the response of cancer patients to checkpoint inhibitors (CPIs). Study, published in Nature Geneticsconfirms these facts in more than 1,400 patients with different types of cancer. These findings provide a framework for defining biomarkers of response to CPIs and suggest future avenues for improving cancer medicine.
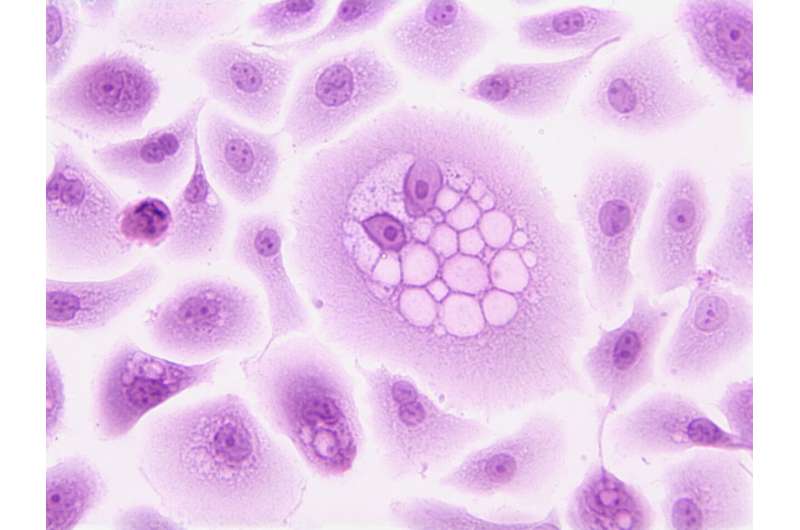
Immunotherapy has revolutionized cancer treatment in recent years by helping the immune system attack tumor cells. However, only 20-40% of patients respond well to immunotherapy, and these rates vary across different types of cancer.
Predicting which patients will respond to immunotherapy and which will not is a very active area of research. Much of the research done so far has focused on the specific characteristics of tumors, their microenvironment, or the patient’s immune system. As a result, which of the proposed biomarkers represent the same factors or how many independent factors influence the effectiveness of this treatment remains unclear.
IRB Barcelona researchers have identified five important, independent factors that determine patient response and survival after receiving checkpoint inhibitors (CPIs), a type of immunotherapy widely used in cancer treatment. These findings provide a reference framework for current and future biomarkers of immunotherapy response.
And, in the future, they could pave the way for major advances in cancer treatment, helping to better identify patients who might benefit from immunotherapy. The results suggest that patients with certain types of tumors that are not currently considered candidates for immunotherapy (such as those with liver or kidney carcinoma) may benefit from this type of treatment.
The team led by Dr. Núria López-Bigas and Dr. Abel González-Perez, from the Biomedical Genomics laboratory at IRB Barcelona, in collaboration with researchers from several international institutions, addressed this issue through a comprehensive analysis of genomic, transcriptomic, and clinical data. from 479 patients with metastatic tumors, who received CPI treatment. This information comes from a public database developed by the Dutch Hartwig Medical Foundation.
Dr. López-Bigas, ICREA researcher at IRB Barcelona explains: “We used an unbiased method to analyze thousands of molecular and clinical parameters and identified five independent factors influencing the response to immunotherapy and the patient’s life.
Five factors, five keys to immunotherapy
Five factors determined by the burden of tumor transformation; effective infiltration of T cells; the activity of transforming growth factor beta (TGF-β) in the tumor microenvironment; previous treatment received by the patient; and the likelihood of tumor spread. These data in different types of cancer are associated with response to CPIs and have been confirmed by the authors in six independent groups, covering a total of 1,491 patients.
- Tumor mutational burden (TMB): Tumors with a high number of mutations tend to produce more neoantigens, making it easier for the immune system to recognize and attack them. TMB has been one of the most studied biomarkers for predicting response to CPIs.
- Effective T-cell penetration: The presence of cytotoxic T-cells within the tumor is essential for the effectiveness of CPIs. This study confirmed that the high penetration of these cells is directly related to a good response to treatment.
- TGF-β activation of the tumor microenvironment: This factor influences the behavior of other cells in the tumor microenvironment. High TGF-β activity can suppress the immune response, indicating a tendency for patients to have poor survival after immunotherapy.
- Previous treatment: Patients who have received prior treatment tend to show a poor response to immunotherapy.
- Proliferative potential of the tumor: Patients with tumors with a high proliferative index, which tend to be aggressive, generally show a poor survival after treatment.
For personalized cancer treatment
These five factors provide a framework for organizing the vast body of current knowledge about biomarkers of immunotherapy response.
Dr. “Until now, most studies have focused on identifying and reporting individual biomarkers, but our results suggest that many of these biomarkers may be – they are different types of the same reasons,” says Dr. González-Pérez.
Furthermore, the researchers showed that a multivariate model combining these five factors allows for more accurate patient grouping than using tumor mutational burden alone (as is often done in clinical practice ), to predict the likelihood that patients will respond to immunotherapy.
This development could have major clinical implications in the future, as it could prevent patients with a low probability of responding from experiencing the side effects of CPIs, which could lead to autoimmune diseases, and can help reduce the cost of treatment.
Certification to international teams
One of the important points of this study is the validation of these five factors in six independent groups of patients with cancer such as lung, colon and melanoma.
“We have confirmed that these factors are important in different types of cancer and different patient populations, thus strengthening their clinical importance. As research continues, new hidden factors may be found in different types of cancer. some cancers or larger groups,” explains Dr. Joseph Usset. , former postdoc at IRB Barcelona who is now at the Oncology Center of Vall d’Hebrón.
The team hopes to have a larger amount of patient data in the future to make more accurate models. The validity of these models for future clinical use should be confirmed by prospective clinical trials. However, this development faces a major challenge, which is the difficulty of obtaining comprehensive and detailed data such as those used in this study.
“This research represents an important step in understanding how different tumor characteristics affect treatment response. In the future, we hope that these five factors will be implemented in clinical practice to guide treatment decisions, “concluded Dr. Lopez-Bigas.
Additional information:
Five hidden factors cause response to immunotherapy, Nature Genetics (2024). DOI: 10.1038/s41588-024-01899-0
Provided by the Institute for Research in Biomedicine (IRB Barcelona)
Excerpt: Study identifies five key factors predicting cancer patients’ response to immunotherapy (2024, September 12) retrieved on September 12, 2024 from https://medicalxpress.com/news/2024-09- key-factors-response-cancer-patients.html
This document is subject to copyright. Except for any legitimate activity for the purpose of private study or research, no part may be reproduced without written permission. Content is provided for informational purposes only.
#study #identifies #key #factors #predict #response #cancer #patients #immunotherapy